
Photo: Getty Images
So by now you know you are supposed to exercise, eat right, and generally live a healthy lifestyle in order to prevent cancer…but we are loving this Health Magazine article outlining the 9 biggest breast cancer breakthroughs in 2013, and the reasons behind why these health and technology advancements are important!
Yes, it’s true: One in eight women will develop breast cancer at some point in her life. Still.
The fact is, “we’ve done a great job of increasing awareness of the disease, but prevention should be the goal for the next decade,” says Marc Hurlbert, PhD, executive director of the Avon Foundation Breast Cancer Crusade. That doesn’t mean experts haven’t made enormous progress: There’s a lot of (very) hopeful news on how to treat the condition more permanently and less painfully, find it at an earlier (and more beatable) stage and even keep from getting it in the first place. Read on for reassurance and empowerment.
A great reason to work out

Courtney Conlogue gets some air in Malibu during B4BC’s Be Healthy. Get Active. Ride! photoshoot.
We know that exercise can reduce your breast cancer risk, but thanks to new research from the University of Minnesota, we’re learning how it may have that effect: “Exercise seems to change the way your body handles estrogen, which often fuels breast cancer,” explains study co-author Mindy Kurzer, PhD. A recent University of North Carolina study has also taught us that even a few hours of physical activity a week can lower your risk, and the more you do, the greater the benefit seems to be (as long as you keep your weight in check, too). “Nearly 30 studies have shown that women who exercise at a moderate to vigorous level for three to four hours per week reduce their risk by 30 to 40 percent,” Kurzer says. “That’s about the same benefit that one gets from tamoxifen—one of our best breast cancer prevention drugs.”
Cancer-fighting food exists

Researchers at the Harvard School of Public Health recently linked vegetable consumption to a lower risk of estrogen receptor-negative (ER-negative) breast cancer, an aggressive type that isn’t fueled by hormones and affects about 15 to 20 percent of women with breast cancer, particularly younger women. Meanwhile, another study revealed that women with higher blood levels of carotenoids—micronutrients found in fruits and vegetables—also had a lower risk of ER-negative cancer. Moreover, berries have been shown in recent studies to reduce the number of ER-positive tumors—the type of breast cancer that affects 70 percent of sufferers, says Harini Aiyer, PhD, a research scientist at the Medical College of Wisconsin in Milwaukee. She adds, “I recommend eating a cup of berries every day.”
New option for at-risk women
Earlier this year, the American Society of Clinical Oncology recommended that doctors discuss the use of exemestane—a drug currently used only for breast cancer patients—with healthy postmenopausal women at increased risk of the disease (say, due to a family history) after a clinical trial showed it reduces the risk of ER-positive breast cancer by up to 73 percent compared with a placebo. Translation: Like tamoxifen and another breast cancer drugcalled raloxifene, exemestane could help fend off cancer in women who are more likely to get the disease.
Breast density matters

Several states require health facilities to notify women if they have dense breast tissue (information you can get from a mammogram). “Having very dense breasts increases your breast cancer risk at least twofold,” says Karla Kerlikowske, MD, a professor in the departments of medicine and epidemiology/biostatistics at the University of California, San Francisco (UCSF). Dense tissue packs more of the types of cells that could possibly promote cancer and also makes it harder to see tumors on a mammogram—one reason mammography doesn’t work as well on younger women, who tend to have denser tissue. If you’re in the dense group, ask for digital mammography, which helps doctors detect abnormalities more easily than with the analog version. (Your doc may recommend an ultrasound or MRI as well.) And use the Breast Cancer Surveillance Consortium’sgroundbreaking new calculator to determine your five-year risk of developing the disease.
A better tech tool
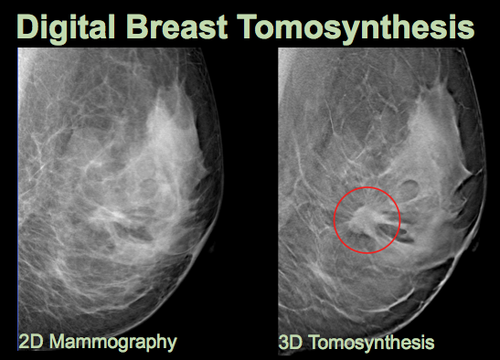
There’s a new, 3-D version of digital mammography, called digital breast tomosynthesis, which can detect more invasive cancers than its 2-D forerunner because it produces a more complete image, particularly for women with dense breast tissue. Though 3-D screening isn’t covered by most insurance yet, “I’m guessing that will change in the next few years as the technology becomes more widely available,” says John Huff, MD, chief of breast imaging at the Vanderbilt University Breast Center. “It’s going to prove to be a powerful technique.”
Safer radiation in less time
For women with small ER-positive tumors—about two-thirds of breast cancer patients, says Holly Pederson, MD, a medical breast specialist at the Cleveland Clinic—studies have shown that undergoing one high dose of radiation during a lumpectomy is as effective as six weeks of postsurgical radiation. Plus, there’s less risk of harming healthy lung and heart tissue. That’s because the radiation is delivered to a 1-centimeter area surrounding the lumpectomy cavity, versus the whole breast. About 40 medical centers in the U.S. offer this approach, called intraoperative radiation therapy.
No cancer left behind

A device called MarginProbe, which was approved by the U.S. Food and Drug Administration (FDA) last year, can be used by surgeons after they’ve removed a tumor to assess whether cells on the tumor’s margins are hard or soft. (Cancerous cells tend to be harder because they contain more collagen.) “Then we can remove additional tissue right there, instead of having the woman return for more surgery at a later date,” says Deanna J. Attai, MD, a breast surgeon at the Center for Breast Care in Burbank, Calif. “It’s incredible.”
Game-changing medications
Kadcyla is one of the most exciting drugs in cancer care because it works like a smart bomb: It delivers chemo straight to the cancer cells and spares the healthy bystanders,” says Erica Mayer, MD, a breast oncologist at the Dana-Farber Cancer Institute in Boston. Designed for women with metastatic HER2-positive breast cancer (a type in which the cancer cells make too much of a protein known as HER2/neu) that has grown despite treatments with chemotherapy and a traditional medication called Herceptin, Kadcyla “extends lives and decreases chemotherapy-related side effects, such as diarrhea and rashes,” Dr. Mayer says. Meanwhile, in April the FDA named a new drug—palbociclib—a “breakthrough therapy,” thanks to a recent study in which it helped improve progression-free survival by 18 months in women with advanced ER-positive, HER2-negative cancer compared with standard chemotherapy alone.
Chemo with less hair loss

The FDA has recently approved a phase II pivotal trial for the DigniCap, a cap worn during chemotherapy that circulates coolant through its inner layer, reducing the delivery of toxins to the hair follicle. In a small pilot study, the device allowed most women with early-stage breast cancer receiving chemotherapy to preserve the majority of their hair. “Most breast cancer research is focused on prevention and treatment, as it should be,” says Hope S. Rugo, MD, lead investigator of the trial and director of the breast oncology and clinical trials education at UCSF. “But if we can enhance patients’ quality of life, too, that’s a good thing.”
**For more on cold cap therapy, check out information by B4BC wellness ambassador, pro snowboarder and breast cancer survivor Megan Pischke and her positive experience with cold cap therapy during treatment.





